CHRONIC OBSTRUCTIVE AIRWAY DISEASE (COPD)
Introduction ;
Chronic Obstructive Airway Disease (COAD), commonly referred to as Chronic Obstructive Pulmonary Disease (COPD), is a progressive and debilitating respiratory disorder that affects millions of individuals worldwide. It is estimated to affect 32 million persons in the United States and is the third leading cause of death in the United States.
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. Symptoms include breathing difficulty, cough, mucus (sputum) production and wheezing. It's typically caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. People with COPD are at increased risk of developing heart disease, lung cancer and a variety of other conditions.
There are two main forms of COPD:
- Chronic bronchitis, In this condition, your bronchial tubes become inflamed and narrowed and your lungs produce more mucus, which can further block the narrowed tubes. You develop a chronic cough trying to clear your airways.
 |
| Bronchitis |
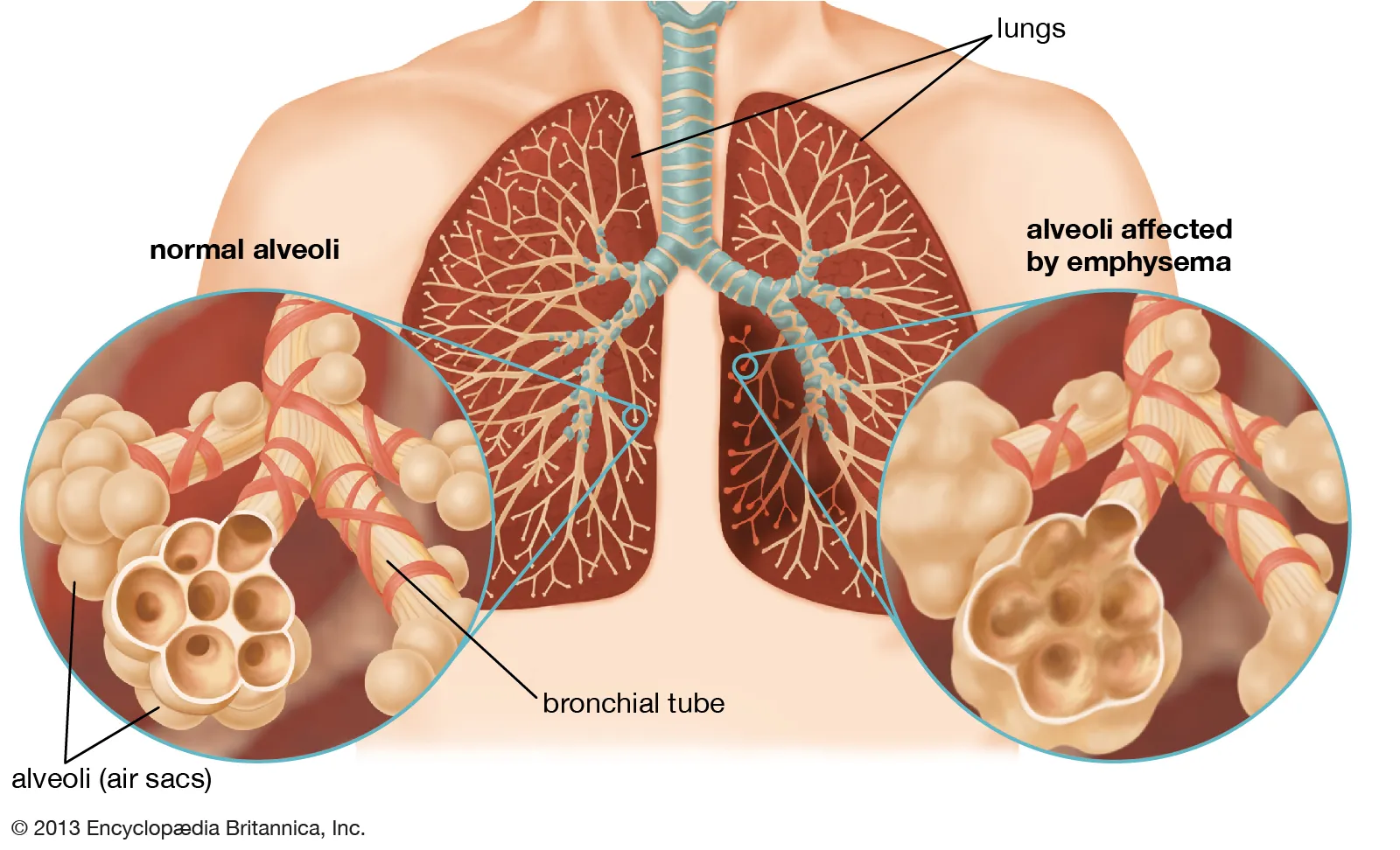
- Emphysema, This lung disease causes destruction of the fragile walls and elastic fibers of the alveoli. Small airways collapse when you exhale, impairing airflow out of your lungs.
 |
| Emphysema |
Most people with COPD have a combination of both conditions. Although COPD is a progressive disease that gets worse over time, COPD is treatable. With proper management, most people with COPD can achieve good symptom control and quality of life, as well as reduced risk of other associated conditions.
Causes ;
Over time, exposure to lung irritants like tobacco smoke or chemicals can damage your lungs and airways. The toxic chemicals in tobacco smoke cause inflammation and irritation of the airways, triggering a cascade of events that lead to structural changes within the lungs .The leading cause of COPD is smoking, however 1 in 4 with COPD never smoked .
- Smoking
- Air pollution
- Alpha 1 Antitrypsin Deficiency
- Occupational exposure
COPD is often referred to as a "smoker’s disease" however although smoking is one of the main risk factors for developing COPD, people who never smoke may also develop COPD. Other risk factors may include:
A history of childhood respiratory infections- Smoke exposure from coal or wood burning stove
- Exposure to secondhand smoke
- People with a history of asthma
- People who have underdeveloped lungs
- Those who are age 40 and older as lung function declines as you age
While these causes and risk factors may increase your risk of developing COPD, people living in poverty and people living in rural areas are more likely to develop COPD. Beyond smoking status, some reasons for the increased risk of developing COPD may include exposures to indoor and outdoor pollutants, occupational exposures and lack of access to healthcare.
Symptoms ;
COPD symptoms often don't appear until significant lung damage has occurred, and they usually worsen over time, particularly if smoking exposure continues.
Signs and symptoms of COPD may include:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- A chronic cough that may produce mucus (sputum) that may be clear, white, yellow or greenish
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Swelling in ankles, feet or legs
People with COPD are also likely to experience episodes called exacerbations, during which their symptoms become worse than the usual day-to-day variation and persist for at least several days.
Talk to your doctor if your symptoms are not improving with treatment or getting worse, or if you notice symptoms of an infection, such as fever or a change in sputum.
Seek immediate medical care if you can't catch your breath, if you experience severe blueness of your lips or fingernail beds (cyanosis) or a rapid heartbeat, or if you feel foggy and have trouble concentrating.
Diagnosis ;
To diagnose COPD, which includes chronic bronchitis and emphysema, your healthcare provider will review your symptoms, ask for your complete health history, conduct a physical exam and look at test results.
After your first visit, your provider will determine your level of severity and create a treatment plan. At each follow up visit, you and your provider will talk about symptoms, risk for COPD flare ups or exacerbations, and make changes to your treatment plan as needed.
History ; Your healthcare provider will take a detailed health history and conduct a physical exam if your provider suspects you may have COPD. You will be asked for some medical history, which should include:
- Current or past smoking history
- Exposure to secondhand smoke; air pollution; prior history working with chemicals, dust or fumes; and a history of childhood respiratory infection.
- History of exacerbations or flare ups including hospitalizations.
- Symptoms such as shortness of breath, chronic cough, or coughing up mucus (sputum or phlegm).
- Family members diagnosed with COPD, alpha-1 deficiency or another chronic lung disease.
- Impact of on how symptoms have changed your daily life. Include changes to your activities or missed work.
- Times when symptoms get worse such as change of season, weather, or other triggers.
- Other comorbidities like heart disease, osteoporosis, anxiety, or depression .
- Testing for COPD ; There are breathing tests or lung function tests your healthcare provider may perform. These breathing tests can be done in your provider’s office while other tests may be done in a pulmonary function testing lab.
- Spirometry ; A spirometry test can diagnose COPD. This helps your healthcare provider see how well your lungs are working.
- Alpha 1 antitrypsin ; Your healthcare provider may order a screening blood test to check the level of alpha-1 antitrypsin in your body.
- Chest X-ray ; A chest X-ray cannot diagnose COPD but can exclude other conditions that have similar symptoms. Chest X-rays can also show changes in your lungs associated with COPD.
- HRCT ; A HRCT may show the type of COPD like emphysema or chronic bronchitis, progression of the disease or severity.
- Arterial blood gases or oximetry ; Oximetry or ABG measures the oxygen level in your blood.
- Lung volume test ; It is to measure the volume of air in the lungs including the air that remains at the end of a normal breath
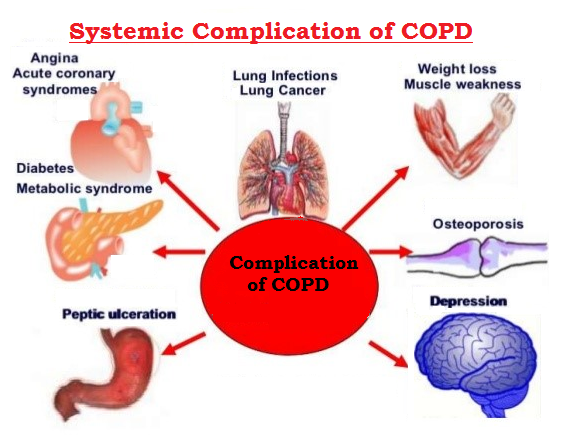
COPD can cause many complications, including:
- Respiratory infections. People with COPD are more likely to catch colds, the flu and pneumonia. Any respiratory infection can make it much more difficult to breathe and could cause further damage to lung tissue.
- Heart problems. For reasons that aren't fully understood, COPD can increase your risk of heart disease, including heart attack
- Lung cancer. People with COPD have a higher risk of developing lung cancer.
- High blood pressure in lung arteries. COPD may cause high blood pressure in the arteries that bring blood to your lungs (pulmonary hypertension).
- Depression. Difficulty breathing can keep you from doing activities that you enjoy. And dealing with serious illness can contribute to the development of depression.
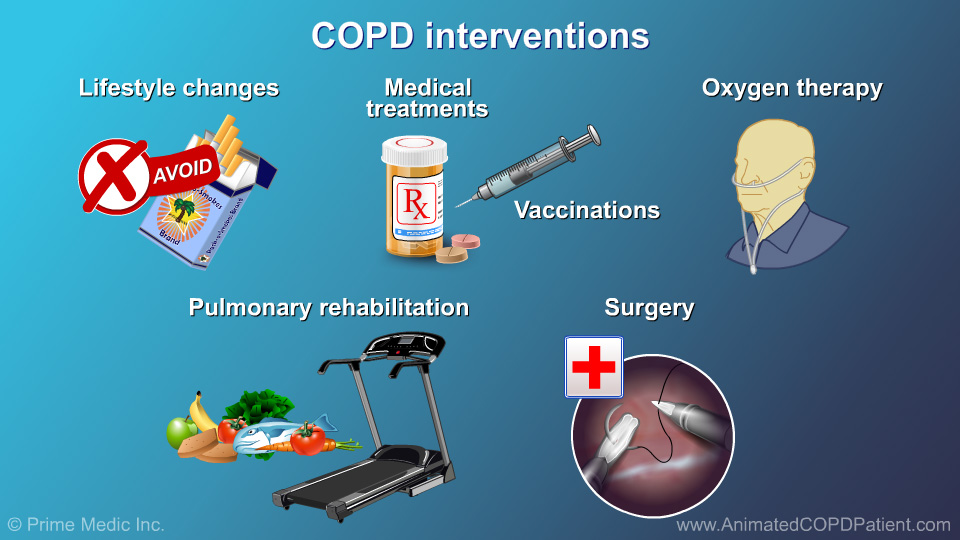
- Life style modification
- Quit smoking
- medications such as Bronchodilators and Inhaled Corticosteroids .
- Pulmonary Rehabilitation programs like exercises , breathing techniques and counseling.
- Supplemental Oxygen therapy.
- Surgical intervention like Lung volume reduction therapy or Lung transplantation.







Comments
Post a Comment